KUALA LUMPUR, Oct 18 — Sometimes stroke patients referred to the programme come in being able to say words like “cat” but are unable to create a full sentence with the word, Dr Mazlina Mazlan said.
After as few as 10 treatments patients can form complete sentences again, the medical specialist consultant in rehabilitation medicine from the University Malaya Medical Centre (UMMC) told Malay Mail.
“I do have a few videos of patients who, before they start the treatment, can say something like ‘cat’, ‘father’, but they cannot form a sentence or explain a story or picture.
“But after 10 sessions, they start to say, ‘The cat sits here’. You can really see the difference in the structure of the words when they start to communicate again,” she said.
Although it is not a hard-and-fast rule that all patients must complete 10 sessions, it is the average based on global studies, she said.
She explained that the 10 sessions can be completed in as quickly as two weeks as sessions are preferably carried out daily on weekdays.
As UMMC is a public health facility, the cost of the initial assessment and 10 treatment sessions is around RM2,000 but it is free for pensioners and civil servants, she added.
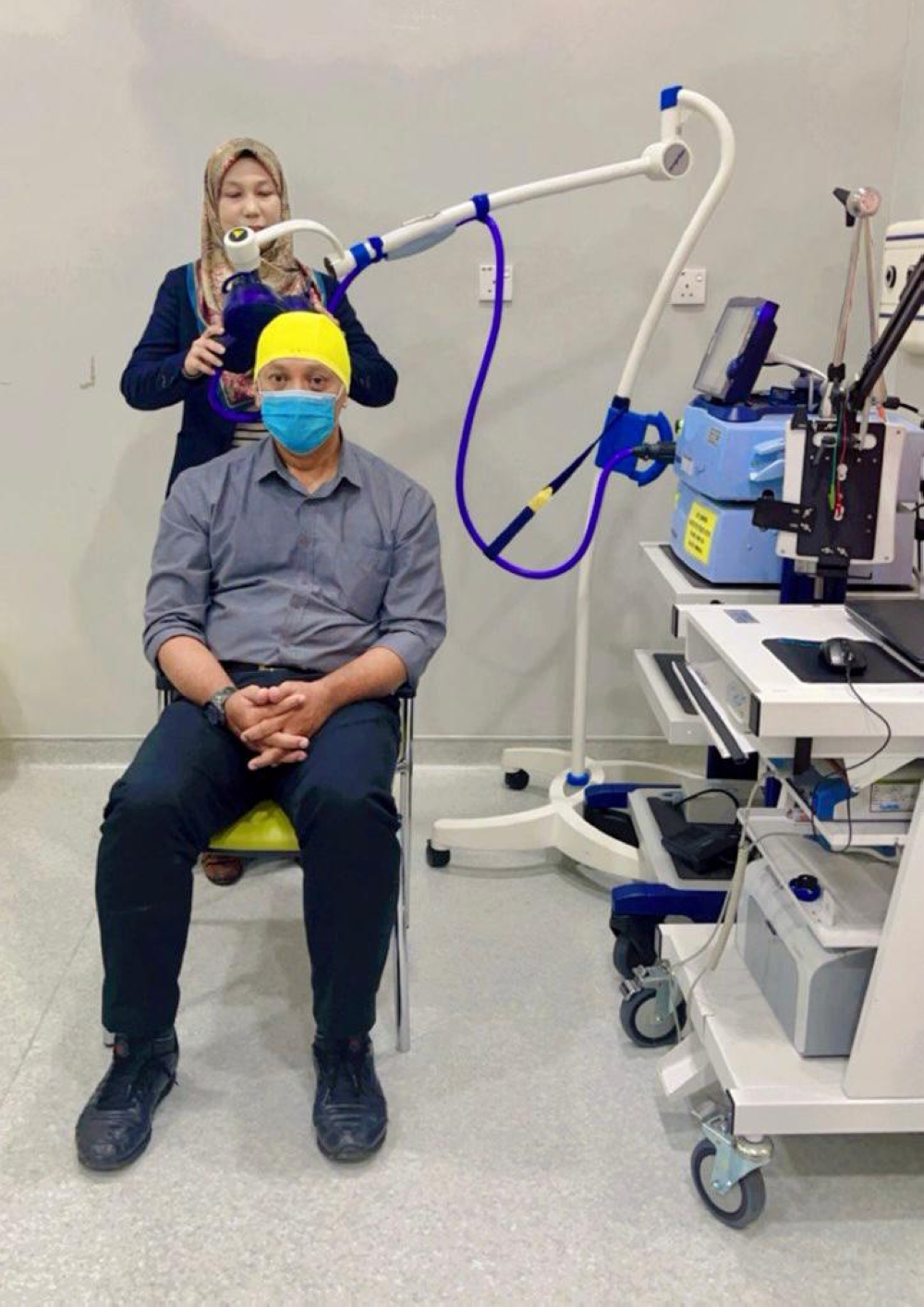
The treatment itself is a non-invasive brain stimulation that takes about 20 to 40 minutes.
“We can either use a weak electrical current to directly stimulate the neurons and make them more active or employ a magnetic field to induce electrical activity in these neurons,” she said.
The former is called transcranial direct current stimulation (TDCS) while the latter is known as transcranial magnetic stimulation (TMS).
Afterwards, within the same day as the treatment, the patient undergoes physical therapy, if their issues lie in motor skills, and speech therapy, if they have issues with language and communication.
The main issue that Dr Mazlina’s team faces is actually a lack of suitable patients.
In the four or five years that the programme had been running, she estimates having seen only 70 to 80 patients undergo it.
Another issue is that patients often come to them later than they’d like.
Dr Mazlina said that the best time for the treatment is within the first three months after having suffered the stroke.
The ideal patient is someone who has suffered a stroke of moderate severity as mild cases are often able to recover on their own while severe cases may have too much widespread damage, she explained.
“Only about 50 per cent of all stroke patients may have a chance to have the benefit of the treatment because they are the ones that are moderately severe meaning that they still have some movement — they will recover with our intensive therapy and we want to enhance that,” she said.
The treatment does have side-effects, she admitted. It was mostly confined to headaches and seizures on the extreme end, though these are extremely rare: the risk is less than 0.01 per cent.
A misconception she often deals with is that patients mistake the treatment for electroconvulsive therapy (ECT).
“The procedure is safe, but patients are sometimes scared because they think of ECT.
“But the patients even have soothing background music, and they just have to sit there and chill,” she said.
The use of electricity to improve brain lesions is nothing new to the medical field as they used electric fish in the time of the ancient Roman empire, she said.
She said that the treatment was originally used to treat major depressive disorder but was found to be effective for stroke patients as well.
Currently, patients come to the centre for treatment through word-of-mouth or referrals, but Dr Mazlina hopes that numbers will increase.
With the experience of the past few years, she and her team are confident in their ability to manage complications and the knowledge the procedure is safe.
“We hope that doctors can refer more patients to us and give chances to those who have a chance to recover.
“Rather than patients being willing to spend hundreds of thousands of ringgit on treatments that are not proven, why not try something that is safe?” she said.






















